Radiobiological Research at the Proton Treatment Center
Research - an undertaking necessary to establish treatment strategies on an experimental rather than empirical basis - underlies all therapeutic uses of the proton beam. At the Proton Treatment Center, this endeavor has two major components: physics studies and radiobiological investigations. The former seek to optimally exploit the capabilities of the proton synchrotron and the beam delivery systems. The latter seek to understand the effects of proton and conventional irradiations in cells, tissues, organs and animals (including humans), particularly in relation to different dose-delivery schedules and different total radiation doses.
One focus of current study is the brain. A primary goal on this avenue of investigation is to identify the sequence of cell population changes that produce the tissue and organ changes, commonly known as late reactions, found months to years after a therapeutic course of irradiation has been completed. A second goal is to identify new time-dose strategies; that is, to develop proton radiation treatment schedules capable of improving cancer control while sparing normal brain tissue.
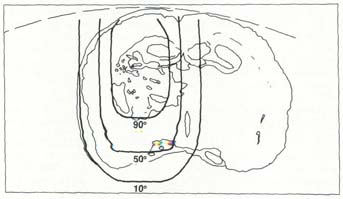
Because of its precision, the proton beam opens up a new dimension in radiobiologic studies in animals. One can confine the dose to a tightly configured volume, sparing adjacent tissue; that tissue then can be used as an effective experimental control. Pictures suggest this capability far better than words. Figure 1 shows a rat immobilized before the beam-delivery nozzle of the 100 MeV proton beam. The illuminated area corresponds to the proton-irradiated segment of the rat's brain; at the edge of the light field, the proton dose is 50 percent of maximum. Figure 2 shows a coronal section of rat brain obtained 11 months after a single proton dose of 40 Gray (4000 rad). Obvious change is seen on the left, including periventricular demyelination, necrosis and cyst formation. The right side, however, appears normal; this segment is used to compare and contrast tissue alterations observed on the irradiated side. Figure 3 shows the isodose lines from the proton beam; the 90 percent line encompasses the area of periventricular necrosis seen in figure 2.
An Innovative Application
When organs are irradiated, radiation biologists try to identify the kinetic changes occurring in the various tissue populations making up those organs. This task is straightforward enough in a two-dimensional laboratory dish containing tissue cultures wherein cells can be counted, but has heretofore been frustrated in the animal. As the radiation dose is increased, it is necessary to identify such changes in the three dimensions of tissue. Researchers from Loma Linda University and Loma Linda University Medical Center have begun experiments designed to yield these important measurements.
In collaboration with Paul McMillan, PhD, professor of anatomy at Loma Linda University, investigators in the department of radiation medicine are applying stereologic techniques to a new problem. The techniques will enable one to calculate, from biopsy specimens, the population changes in three-dimensional tissue volumes and, by extension, in organs. Although stereologic techniques are well-known in other disciplines, such as anatomy and geology, their application in radiation biology is being pioneered at Loma Linda.
With the assistance of Joseph Thompson, MD, of the section of neuroradiologoy, and Andrew Kennedy, MD, of the LLUMC house staff, radiation medicine investigators are performing histologic analyses to document and interpret changes observed on magnetic resonance images. This work seeks to determine the degree to which histologic changes can be inferred from image changes, and thus, the degree to which MRI can be employed as a measure of the brain's response to irradiation. If imaging results can be correlated precisely with histologic events, the images may be useful as monitors of therapeutic response. Thus far, the effort has enabled the investigators to identify graded changes in the brain following different total doses and different fractions of proton irradiation.
The immediate goal of this three-dimensional work is to test the hypothesis that the microvasculature is the tissue most sensitive to irradiation; that damage to the microvessels results in changes in other tissues, which in turn produce the well-known long-term sequelae. Two-dimensional measurements of the microvasculature, made on microscopic sections, do not sufficiently describe postradiation population effects; nor do they show the relationships within or between the components of tissue volumes. Using a special staining technique they developed, however, and employing computer-assisted three-dimensional reconstructions, Dr. McMillan and Marie-Helene Archambeau are evaluating the changes in brain microvessels and are comparing those changes observed with the same vessels in unirradiated brain tissue.
Other Research Areas
Researchers are measuring the dose response of V-79 (murine) cells, with the aim of characterizing proton beams of different sizes and energies. James Robertson, PhD, of East Carolina University, is conducting these studies. He has determined the dose survival of V-79 cells for the horizontal proton beam, and is now obtaining the same data for the more energetic gantry beam. These data are being compared with data from conventional radiation therapy machines, to determine the relative response of cells to similar doses from proton and photon radiations. From these data it will be possible to specify the efficiency of the protons.
In another area of concern, LLU and LLUMC investigators are measuring the different tissue and organ responses patients may have after conventional radiation treatment. The results obtained at LLU and LLUMC are compared with the same data from other clinicians, to assure that the responses are both uniform and as expected. Animal models are then employed to quantify the dose response of tissues to new time-dose schedules and to total doses of protons. The results enable researchers to evaluate what may be expected to occur in similarly irradiated normal human tissues.
New studies have been undertaken to determine the true boundary between normal brain and tumor contained within it. In collaboration with Boleslaw Liwnicz, MD, of the department of pathology, Robert Iacono, MD, of neurosurgery, and Joseph Thompson, MD, of neuroradiology, researchers from the department of radiation medicine are mapping this boundary by correlating the histologic changes seen on stereotactic biopsies, with observations detectable on magnetic resonance images.
As the work progresses, it is shared with clinicians. Researchers participate in the Pediatric Tumor Board and, when indicated, in Children's Cancer Group studies. The purpose of these contacts is to maintain a dialogue between research efforts and clinical realities, so that each may influence the other as needed. Clinicians and researchers keep each other aware of progress, as well as problems.
LLUs proton beam capability provides researchers with a new tool for many investigations. Michael Moyers, PhD, of medical physics, and Michael Kirby, PhD, of pediatrics, are applying a unique perspective in using proton beams as a tool to define tissue function. They are developing proton microbeams to study the effects of radiation-injured cells on physiologic processes. The proton beam's precision makes it feasible to irradiate critical brain centers (nuclei) of a few cells, to estimate their role in a process such as vision.
Establishing a Foundation
Proton-beam irradiation is not experimental. Its clinical utility has been demonstrated for over forty years, and to date many more than 10,000 patients have been treated with proton beams at research facilities around the world. Loma Linda University Medical Center, however, has the potential for serving patients with disease in anatomic sites heretofore not treatable with protons, because it has the first accelerator and facility in the world designed for treating patients in a clinical setting. The facility has been designed to exploit proton beams as fully as possible, and to integrate that exploitation with clinical realities. Accordingly, the Proton Treatment Center is located adjacent to, and employs the services of, diagnosticians, researchers, and other clinicians. The research effort is part of the integrated activities expected of a referral cancer center.
This increased potential available with proton-beam therapy demands research to optimally exploit the potential. The department of radiation medicine's research program seeks to aid in this scientific effort by undertaking carefully designed and meticulously performed investigations, to apply new tools to old problems in such a way that clinical advances may build on a sound and objective basis.